Introduction
When most people hear the word schizophrenia, their minds immediately jump to dramatic symptoms often portrayed in films and media. Hallucinations, or delusions for example. These are known as positive symptoms, and while they can be distressing, they’re often treatable with medication.
Before we continue, with the context of this article’s topic in mind, the words “Positive” and “Negative” do not mean “Good” and “Bad”. Instead they carry the meaning more like “Additive” and “Subtractive”.
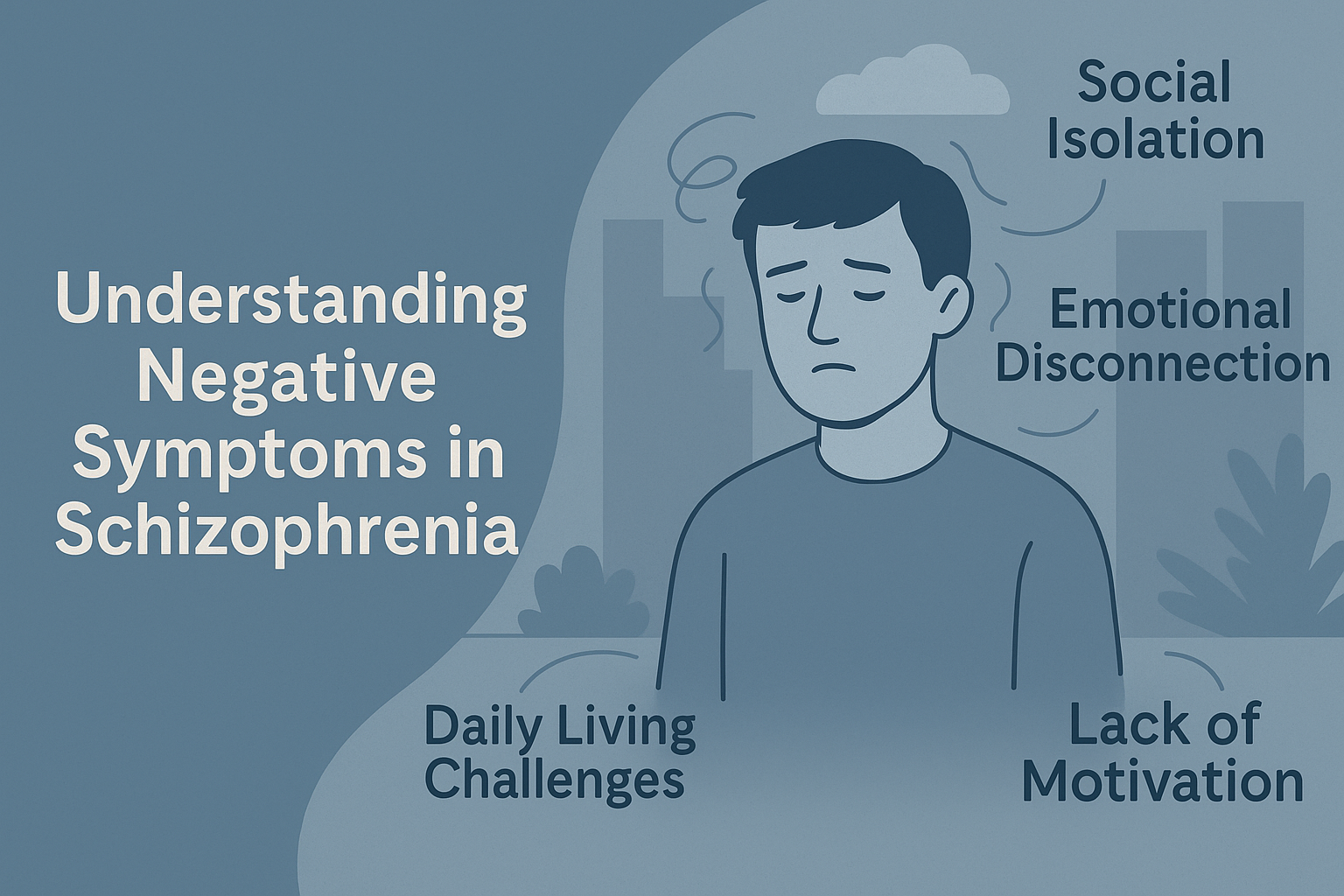
What many people don’t know is that schizophrenia also brings another set of challenges, ones that are far less visible but often more disabling in the long run. These are the negative symptoms. Unlike positive symptoms, which add experiences that shouldn’t be there (like hearing voices), negative symptoms involve the loss of normal abilities and behaviours.
For families, carers, and even professionals, these symptoms can be confusing and frustrating. Why does your loved one seem withdrawn? Why don’t they want to do things they once enjoyed? Why do they seem emotionally “flat”? Understanding these questions is key to providing the right support.
What Are Negative Symptoms?
Negative symptoms refer to the absence or reduction of typical behaviours, emotions, and motivations that are essential for daily functioning. They are not about being “negative” in attitude but about missing aspects of normal mental and emotional life.
Unlike the dramatic and visible nature of positive symptoms such as hallucinations, these changes are subtle and often misinterpreted as laziness or lack of interest. In reality, they stem from complex neurological processes that impact motivation, reward, and emotional regulation.
Here are the main categories:
- Affective Flattening – A noticeable reduction in emotional expression. The person might speak in a monotone voice, show little facial expression, or seem “blank” even during emotionally charged moments.
- Alogia – Limited speech. Conversations become short and minimal, not because of rudeness, but due to difficulty generating thoughts or expressing them.
- Anhedonia – Loss of pleasure in activities that used to bring joy. Even favourite hobbies or social outings may hold no appeal.
- Avolition – A lack of motivation to initiate or sustain activities. Everyday tasks like showering, cooking, or tidying up can feel overwhelming.
- Asociality – Withdrawal from social interactions. Relationships may fade because engaging with others feels exhausting or pointless.
These symptoms are not a choice. They reflect deep changes in brain functioning that make previously simple tasks feel like climbing a mountain. Unfortunately, their subtle nature means they’re often overlooked by family, friends, and even healthcare providers.
Recognising them early is key to offering the right support, building realistic expectations, and creating an environment that encourages small, sustainable steps toward engagement and recovery.
Why Are Negative Symptoms Misunderstood?
Unlike hallucinations or delusions, negative symptoms aren’t obvious. They don’t make headlines or feature in dramatic TV scenes. Instead, they look like “quiet suffering.” This invisibility leads to misinterpretation and stigma.
Many families mistake these symptoms for laziness or apathy:
- “He just doesn’t care anymore.”
- “She’s being antisocial.”
In reality, negative symptoms stem from neurological disruptions in areas of the brain responsible for motivation, reward, and emotional processing. Think of it like a car with an empty fuel tank: the engine (the person) is still there, but there’s no energy to make it move.
Negative symptoms are also commonly confused with depression or side effects of medication. While overlaps exist, they are distinct issues requiring different strategies. Unfortunately, this misunderstanding often delays effective intervention, leaving the individual and their family frustrated and disconnected.
Impact on Daily Life
The effect of negative symptoms can be profound and far-reaching. Unlike positive symptoms, which may come and go, negative symptoms often persist over time and quietly erode a person’s quality of life.
These changes ripple outward to families, friendships, and work environments. While positive symptoms might draw attention due to their disruptive nature, negative symptoms often hide in plain sight, gradually dismantling routines and relationships.
Here’s how they commonly manifest:
- Social Isolation – Friends drift away. Conversations become rare. Loneliness sets in. What once felt effortless—chatting over coffee, attending gatherings—becomes an exhausting mental task.
- Daily Living Challenges – Hygiene, cooking, cleaning—all can fall by the wayside, not out of choice but due to lack of mental energy and motivation. Even something as small as brushing teeth can feel overwhelming.
- Employment Difficulties – Holding a job becomes difficult when motivation and focus are diminished. Tasks pile up, and performance issues may be misread as disinterest rather than symptoms.
- Emotional Disconnection – Loved ones may feel shut out because emotional warmth seems absent. Smiles, laughter, and shared moments fade, creating misunderstandings and tension.
These struggles can be devastating. Many individuals desperately want to engage with life, but their internal resources simply aren’t there. This disconnect often leads to feelings of guilt, frustration, and hopelessness, compounding their mental health challenges.
Families, too, can feel helpless or even resentful, not realising that these behaviours aren’t a choice. Understanding the true nature of negative symptoms is the first step toward offering compassion and practical support that can make a real difference.
Why Are They So Hard to Treat?
Medication, while life-changing for positive symptoms, often does little for negative symptoms. Antipsychotic drugs primarily target dopamine pathways involved in hallucinations and delusions, but negative symptoms involve broader brain networks affecting motivation, pleasure, and cognition.
Current research explores new medication options and therapies, but for now, psychosocial interventions remain the backbone of treatment. This includes structured routines, behavioural activation (gradually reintroducing rewarding activities), and skills training.
How Residential Care Can Help
This is where dedicated residential support changes lives. Negative symptoms thrive in environments lacking structure and encouragement. In contrast, care homes like Serendipity create predictable, supportive routines that reduce stress and gently promote engagement.
Some key strategies:
- Structured Daily Routines – Predictability is calming and helps reduce decision fatigue. Having consistent meal times, scheduled activities, and gentle reminders creates a sense of order that can anchor individuals who might otherwise feel adrift.
For someone struggling with avolition, knowing what comes next can be the difference between completing a task and avoiding it altogether.
- Engagement Activities – Activities like art, gardening, or cooking groups provide stimulation in a non-threatening way. These go beyond hobbies, and offer a sense of accomplishment and rekindle interest in the world.
When carefully chosen and introduced at the right pace, such activities can bypass the weight of apathy and spark small moments of joy or curiosity.
- Supportive Social Opportunities – Traditional social situations can feel overwhelming for someone with negative symptoms. Low-pressure group interactions, such as a shared tea break or collaborative art session, allow social skills to rebuild gently.
The goal isn’t forced participation but creating safe, welcoming spaces where connection feels possible without pressure.
- Skilled Observation – Negative symptoms often shift slowly, making it easy to miss early signs of improvement or decline. Staff trained to notice subtle changes like a slight increase in eye contact, a willingness to join a group, or conversely, a retreat into isolation, can adapt care plans before issues escalate. This attentiveness is vital for long-term stability and progress.
The goal isn’t to force participation but to create opportunities for success. Small wins that rebuild self-esteem and motivation are the goal.
How Families Can Support Loved Ones
Family support is vital, but it requires understanding and patience. Here are practical tips:
- Avoid Criticism – Comments like “Try harder” or “You’re being lazy” are harmful. Negative symptoms are not a choice. Criticism can deepen feelings of shame and withdrawal, making recovery even harder.
- Encourage Small Steps – Instead of “Let’s go out for the day,” try “Would you like to sit in the garden for 10 minutes?” Starting small helps build confidence and prevents the person from feeling overwhelmed.
- Celebrate Progress – Even tiny improvements matter. Acknowledge them warmly. Positive reinforcement can motivate further engagement and show the person that their efforts are valued.
- Maintain Connection – Even when responses are minimal, your presence and consistency provide security. Silent companionship can still offer comfort and reduce feelings of isolation.
- Seek Education – Learn about negative symptoms to adjust expectations and reduce frustration. Understanding the condition helps caregivers respond with empathy rather than impatience.
Why This Matters
Negative symptoms can be more disabling than positive symptoms. They erode quality of life and independence and can strain relationships to breaking point. Without targeted support, these symptoms often persist for years.
At Serendipity Care, we understand that supporting someone with schizophrenia isn’t just about controlling psychosis—it’s about nurturing the whole person. Our homes provide structured, compassionate environments where individuals can stabilise, reconnect, and rediscover meaning in life.
If you’d like to learn more about how we support people with complex mental health needs, contact us today. Together, we can build a future where no one faces this silent struggle alone.