Uncategorised
Highlights from April 2025


High-Functioning Depression and Anxiety – A UK-Focused Analysis
1. What is High-Functioning Depression and Anxiety?
High-functioning depression is not an official diagnosis, but the term describes individuals who experience depressive symptoms yet manage to maintain daily responsibilities medicalnewstoday.com priorygroup.com.
Depression

In clinical terms, it often aligns with persistent depressive disorder (dysthymia) – a chronic, mild form of depression. Unlike a major depressive episode which is severe and usually obvious, dysthymia involves a continuous low mood that may appear “normal” to others because the person’s symptoms are less debilitating medicalnewstoday.com priorygroup.com.
For example, someone with high-functioning depression might feel sad, fatigued, and pessimistic, but still go to work and socialize, albeit with great internal effort northernhealthcare.org.uk. They fulfill obligations while feeling empty or “in a funk” internally, so their struggles often remain unseen counselling-directory.org.uk.
Anxiety

High-functioning anxiety likewise refers to individuals who experience chronic anxiety (such as excessive worry, tension, and overthinking) but outwardly cope well. It is not a formal diagnosis in manuals like DSM-5, but a descriptive term. People with high-functioning anxiety typically meet many symptoms of generalized anxiety disorder (GAD) – for instance, constant worry or inner turmoil – yet they appear calm and successful externally bupa.co.uk counselling-directory.org.uk.
The key difference is one of outward impairment: Generalised Anxiety Disorder is usually diagnosed when anxiety causes significant distress or interferes with daily life (e.g. struggling to work or socialize) nhs.uk. By contrast, those with high-functioning anxiety often mask their distress and continue to perform at a high level, so they might not seem impaired even though they feel intense anxiety internally bupa.co.uk.
Current Understanding in The UK
In short, the “high-functioning” label means the person’s mental health issues are real but hidden behind a façade of normalcy.
Current understanding in the UK recognises that these high-functioning forms are common yet underdiagnosed. Many Brits experience what NHS and mental health charities term “mixed anxiety and depression,” a blend of milder symptoms that doesn’t neatly fit severe diagnostic categories. In fact, mixed anxiety-depression is Britain’s most common mental health condition, affecting about 7–8% of people any given week mentalhealth.org.uk mind.org.uk
2. The Mask of Productivity
People with high-functioning mood disorders often wear a “mask” of productivity and positivity to hide their internal pain. There are powerful psychological and social reasons behind this coping strategy.
The Role of Stigma
Stigma and misunderstanding play a big role – sufferers fear being judged or not taken seriously because outwardly they seem “fine.” They may think others won’t understand their struggles if they admit to them. For instance, a person might carry on as normal and avoid asking for help because they worry those around them will not understand what they’re going through northernhealthcare.org.uk.
Individual Personalities
Personality traits and coping styles also drive the mask of productivity. High-achieving or perfectionistic individuals tend to tie their self-worth to success and competence. Paradoxically, when anxiety or depression strikes, they often respond by overcompensating – working even harder and striving for even more perfection to maintain control.
As one psychologist observed, many executives and high performers who notice mental health “red flags” will “put their foot on the gas” and push themselves harder, using work as an unhealthy coping mechanism bupa.co.uk.
Pushing Through it
In their minds, slowing down or showing struggle isn’t an option, so they double down on productivity to escape or “outrun” their feelings. This performative coping can fool people around them (and sometimes the individuals themselves) into thinking nothing is wrong.
A UK psychotherapist notes that such a person might “mask their symptoms or become highly performative to disguise the depression,” causing others to misread the signs as mere personality quirks (like being moody or irritable) rather than a mental health issue counselling-directory.org.uk.
In other words, they perfect the art of appearing excessively together – staying on top of work, keeping social commitments, and never letting the mask slip.
3. Emotional Exhaustion and Burnout
Maintaining a façade of normalcy despite depression or anxiety is mentally and physically exhausting. Over time, the effort of pretending to be okay – smiling, performing, and suppressing negative emotions – drains one’s energy reserves. Many high-functioning individuals report perpetual fatigue.
For example, even if they appear productive, they might privately feel tired all the time, struggle with sleep, and find that completing routine tasks requires immense effort northernhealthcare.org.uk.
“Burning the Candle at Both Ends”

Essentially, they are burning double the fuel: one part of them deals with the usual demands of work and life, while another part constantly battles or conceals their internal symptoms. This continual internal battle can lead to emotional exhaustion, where the person feels “empty” or numb. They may fulfill roles – employee, parent, friend – on autopilot, all the while inching closer to burnout.
What is Burnout?
Burnout is a state of chronic stress and exhaustion, and high-functioning sufferers are at high risk because they rarely give themselves permission to rest or recuperate. The long-term impact on mental health can be severe. By pushing through depression or anxiety without adequate support, individuals often exacerbate their conditions.
What starts as mild, hidden depression can deepen over the years. Psychotherapists note that relentless stress (for instance in a high-pressure job) can “easily turn to burnout,” which in turn provokes secondary mental health problems, such as anxiety and depression becoming chronic counselling-directory.org.uk.
4. The Danger of Misdiagnosis and Lack of Support
High-functioning individuals with mood disorders are often overlooked or misdiagnosed by healthcare providers, meaning they don’t get the support they need. One reason is that they don’t fit the stereotype of someone who is depressed or severely anxious.
A GP appointment in the UK may last only 10 minutes, and if the patient is well-dressed, employed, and saying they’re “fine, just a bit tired,” the deeper issue can be missed.
Many mask their symptoms so well that even doctors and therapists struggle to spot the distress counselling-directory.org.uk. In mild cases, depression might be brushed off as just a personality trait. As one counsellor notes, the subtle symptoms might be excused as someone “just being moody” or pessimistic, rather than recognized as depression counselling-directory.org.uk.
The UK’s Awareness Gap
In the UK, awareness of this gap is growing. Experts are calling for better screening and understanding – for example, realising that high performance does not equal high mental health. There is recognition that workplaces and GPs should be alert to those who appear well but report persistent low mood or anxiety.
The danger of not addressing these cases is clear: without proper support, high-functioning depression can worsen until it becomes debilitating, and high-functioning anxiety can escalate into panic attacks or breakdowns. In the worst cases, people who seemed to “have it all together” might reach a crisis point (such as contemplating self-harm) with little warning, because their pain was hidden. This makes improved recognition essential.
Bridging the support gap – through proactive mental health check-ups and encouraging honest conversation – is an ongoing challenge for the UK’s healthcare system, which currently leaves many high-functioning individuals to “suffer in silence”.
5. Coping Mechanisms and Treatment Options
Despite these challenges, there are effective strategies and treatments to help individuals manage high-functioning depression and anxiety. Coping mechanisms typically involve both personal self-care approaches and leveraging support networks. Mental health experts emphasize first acknowledging the problem – one must accept that they are struggling and it’s not “normal” to feel persistently sad, anxious or empty northernhealthcare.org.uk.
Learning to Talk About It

This mental shift is important for high-functioning people who often downplay their feelings. Rather than judging oneself for not coping “perfectly,” it’s crucial to recognize the need for care. Next, sharing feelings with someone trusted can relieve the pressure. This might mean opening up to a close friend or family member about what’s really going on behind the mask.
Many find that simply talking about their low days or worries is cathartic and makes it easier to seek further help. If talking is hard, writing in a journal or expressing emotions through art can also be a release northernhealthcare.org.uk. The key is not to carry the burden alone.
Physical Activity
In terms of day-to-day coping, maintaining healthy routines and self-care practices can significantly improve mood and stress levels. Regular physical exercise is one of the simplest and most effective tools. The NHS notes that exercise is a proven treatment for mild depression and can boost mood nhs.uk.
Even a daily walk or some form of movement can reduce anxiety and improve sleep. Many doctors will actually “prescribe” exercise or refer patients to group activity programs as a part of treatment for mild depression nhs.uk.
Make Time for Relaxation
Other self-care practices include mindfulness and relaxation techniques. Learning mindfulness meditation, deep-breathing exercises, or yoga can help calm the overactive mind and relieve anxiety. In fact, a notable portion of high-functioning individuals turn to these methods: one survey of executives with high-functioning anxiety found 44% used relaxation techniques and 33% practiced mindfulness/meditation to cope bupa.co.uk.
Alongside self-help strategies, there are effective treatment options available via the NHS and privately. The first port of call is usually your GP (General Practitioner). It’s advisable to clearly communicate your symptoms to the GP – even if you function well, explain the low mood, anxiety, or exhaustion you feel internally.
Therapy
GPs in the UK can offer advice and also refer you to therapy services. The NHS provides Talking Therapies (previously called IAPT – Improving Access to Psychological Therapies) for common mental health problems like depression and anxiety. You can be referred by your GP or even self-refer to these services in your area northernhealthcare.org.uk nhs.uk.
Cognitive Behavioural Therapy (CBT) is one of the most commonly recommended therapies – it helps you identify and reframe unhelpful thought patterns and gradually change behaviors. For high-functioning individuals, CBT can be very useful to challenge perfectionism, negative self-talk, or catastrophic thinking associated with anxiety. Other therapy modalities include counselling (providing a space to talk and be heard), interpersonal therapy (focusing on relationships), or even newer approaches like mindfulness-based therapy. Counselling or therapy is highly beneficial – it provides tools to manage symptoms and also a private outlet to finally drop the “I’m fine” mask counselling-directory.org.uk.
Highlights from March 2025

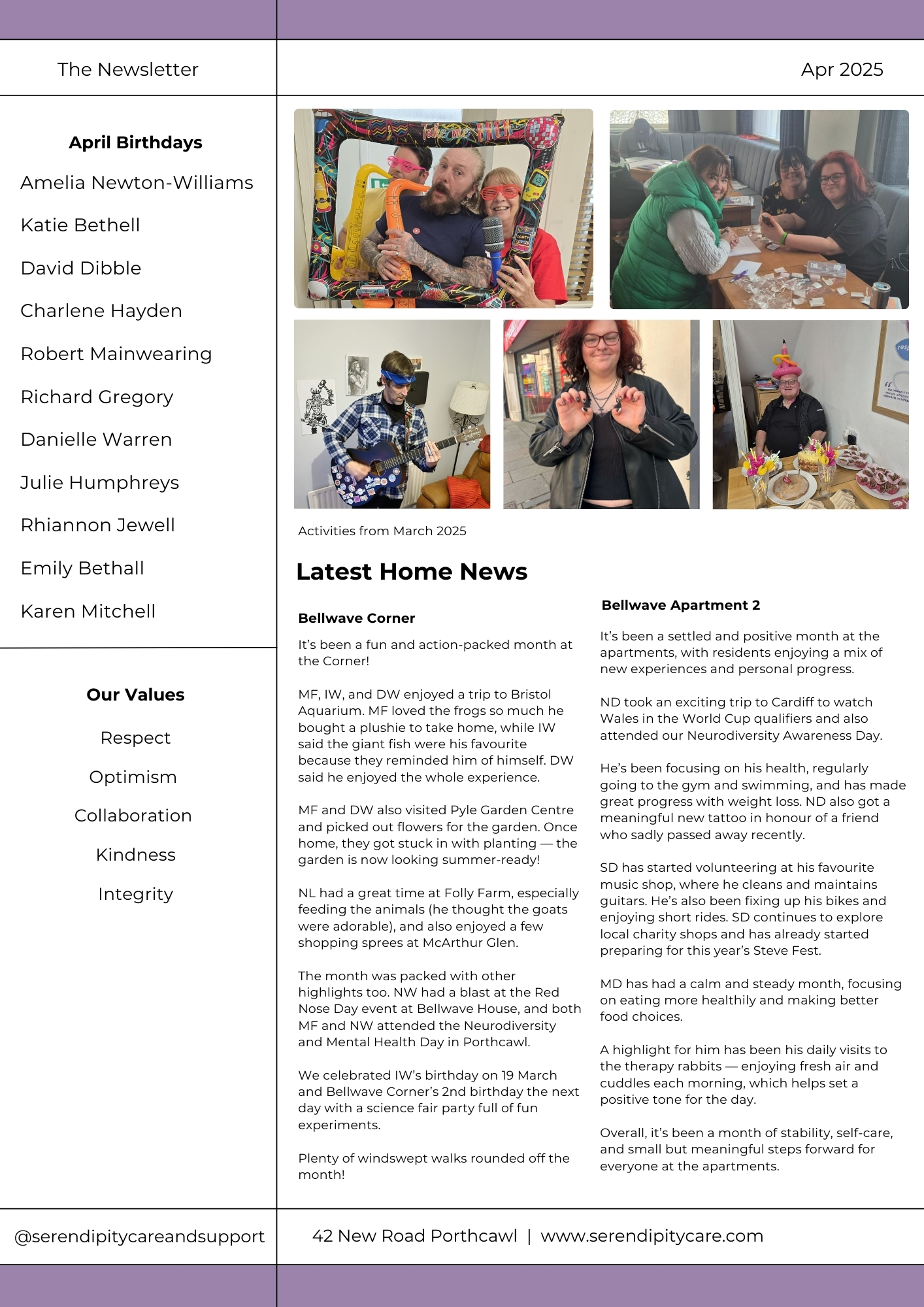
Highlights from February 2025

The Role of Family and Caregivers in Schizophrenia Treatment and Recovery
Introduction
Living with schizophrenia presents challenges that affect not only the individual but also their families and caregivers. The journey toward stability and recovery requires a strong support system built on understanding, empathy, and effective communication.
Families play a vital role in helping their loved ones navigate symptoms, adhere to treatment plans, and build a fulfilling life. At the same time, caregivers must also manage their own well-being to sustain long-term support.
In this article, we explore the many facets of caregiving for individuals with schizophrenia—offering insights into fostering resilience, promoting autonomy, and maintaining a healthy, balanced approach to care. Through a focus on compassion and collaboration, families can become a pillar of strength in their loved one’s recovery journey
Understanding the Diagnosis
The most foundational step to providing meaningful care and support is: understanding.
Receiving a schizophrenia diagnosis can be an overwhelming experience, not just for the individual but also for their family. The condition is complex, often misunderstood, and surrounded by misconceptions.
It’s crucial for families to take time to understand what schizophrenia is—its symptoms, potential triggers, treatment options, and long-term prognosis.
Oftentimes there has been a lot of struggles before a diagnosis is ever given. It’s important to take a moment to reflect and see those struggles through a new lens. It’s at this time when a bit of research will go a long way.
Educating oneself and the broader family circle reduces fear and confusion, creating a foundation for empathy and informed support. Resources such as mental health charities, healthcare providers, and support groups can offer valuable guidance during this process.
The Impact of Stigma

Stigma remains one of the greatest barriers to mental health recovery. Individuals with schizophrenia and their families often face discrimination, which can foster feelings of isolation and shame.
Family members may hesitate to seek help or share their struggles for fear of judgment. It can help to remember that understanding around mental illness, while still lacking, is definitely improving. People have become more accepting of the fact that not all brains function in the same way. Still, stigma and misconceptions can be deeply ingrained, even (and sometimes especially) in those who are most affected by them.
Fighting stigma starts within the home. Families that openly discuss mental health, challenge myths, and emphasise their loved one’s dignity can provide a powerful buffer against external negativity. Over time, this support fosters resilience, encouraging the individual to remain engaged in treatment and social activities.
Establishing a Supportive Environment
A stable, nurturing home environment is essential for individuals with schizophrenia. Routines can provide a sense of predictability, which helps reduce anxiety and prevent episodes. This might include structured meal times, regular sleep schedules, and planned activities to maintain a sense of purpose.
A not-untypical scenario might look like this:
A young woman is living with schizophrenia. Her family discovered that keeping a regular morning routine—breakfast at 8am, followed by a walk around the block—helped her start the day with less agitation. However, there were days when she struggled to get out of bed, her energy drained by negative symptoms such as apathy and fatigue. On those days, her parents learned to gently modify the routine, offering to have breakfast together later or suggesting shorter, less demanding activities. Over time, this combination of structure and compassion helped Sarah feel supported without being overwhelmed by expectations.
For many families, the process of finding that balance involves trial and error. This process is not always smooth and it can put a real strain on the mental wellbeing of the primary caregivers.
Support groups often share similar stories, underscoring that setbacks are normal and that flexibility can prevent feelings of failure for both the individual and the caregivers. Encouraging participation in low-pressure activities, like art or gardening, can offer an outlet for creativity and emotional regulation on more challenging days.
However, flexibility is also important. Mental health can fluctuate, so families should learn to adapt routines to accommodate their loved one’s changing needs. A balance between structure and compassion helps build a calm atmosphere that supports recovery.
Communicating Effectively

Clear, compassionate communication is a cornerstone of effective support. People with schizophrenia may experience cognitive difficulties, including trouble processing information or maintaining focus. Families can help by simplifying conversations, using direct language, and offering gentle reminders.
Effective communication is a deliberate and conscious effort, it requires practice and patience. It is easy to fall into patterns of communication that can be unhelpful. A stressed mind defaults to low resistance patterns of thought. This can sometimes mean letting frustration get the better of us, expectations need to be realistic and empathy should abound.
Active listening is equally important. Instead of rushing to provide solutions, families should listen without judgment, showing empathy and patience. During periods of psychosis or heightened anxiety, communication strategies such as maintaining calm body language and avoiding confrontation can help de-escalate tensions.
Recognising and Managing Triggers
Understanding and managing triggers is a crucial part of preventing relapses. Stress, substance use, and lack of sleep are common triggers for schizophrenia symptoms. Families can work with healthcare professionals to identify specific triggers and develop strategies to mitigate their impact.
Early warning signs, such as withdrawal, increased agitation, or disrupted sleep patterns, should also be monitored. When caught early, intervention can prevent small issues from escalating into a full-blown crisis.
Caregiver Burnout and Self-Care
This is an extremely important section, we realise it can be a sensitive topic but it’s at the core of everything else. An individual suffering with such a debilitating condition such as schizophrenia can have some seriously bad outcomes if the support is not there. The better the support, the better the outcomes, generally speaking of course.
In order to offer the kind of support necessary, the caregiver must be at their best within themselves. This is hard enough to manage without the added challenge and responsibility of caring for someone else. When the person requiring care has a condition as severe as schizophrenia, the difficulty goes up once again.
Caring for someone with schizophrenia can be physically and emotionally taxing. Many caregivers face burnout, which can manifest as exhaustion, irritability, and feelings of hopelessness. It’s vital that caregivers appropriately prioritise their own well-being.
Practices such as regular exercise, socialising, and engaging in hobbies help caregivers recharge. Professional counselling or joining a caregiver support group can also offer valuable emotional support. By taking care of themselves, caregivers are better equipped to provide sustainable care for their loved ones.
The bottom line is that caring for an individual with a complex condition requires you to be “switched on” a lot of the time. This in itself can be exhausting. Recognising the importance of giving yourself time to “recharge” is crucial.
Balancing Autonomy and Support
While people with schizophrenia may need assistance, maintaining their autonomy is crucial for long-term recovery. Over-reliance on family members can hinder the development of coping skills and self-esteem.
Families should encourage their loved one to make decisions about their treatment and daily life, even if those decisions seem small. Offering choices—such as what to eat, how to spend time, or which activities to pursue—fosters a sense of control and independence.
Crisis Management
Despite best efforts, crises may occur. Episodes of acute psychosis or severe distress require a clear plan to ensure safety. Families should work with healthcare providers to develop a crisis plan, which may include emergency contact numbers, medications, and de-escalation strategies.
Preparation can make crises less overwhelming. By rehearsing scenarios and discussing the plan with all household members, families can respond more effectively when urgent situations arise.
Emotional Healing and Forgiveness
Schizophrenia can strain family relationships, particularly when symptoms lead to misunderstandings or hurtful behaviour. Rebuilding trust after challenging episodes takes time and patience.
Families can promote healing by acknowledging the difference between the person and their symptoms. Open conversations about forgiveness, boundaries, and emotional needs can help repair fractured relationships, allowing both the individual and their family to move forward together.
The Importance of Patience and Long-Term Commitment
Recovery from schizophrenia is a marathon, not a sprint. Symptoms may ebb and flow over time, and setbacks are normal. Families that understand this long-term perspective are better able to provide consistent support without becoming discouraged by temporary relapses.
Maintaining hope, flexibility, and realistic expectations helps create an environment where gradual progress can be celebrated. Families should remind themselves that every small step forward—whether it’s sticking to a routine or attending therapy sessions—is a victory.
Conclusion: How Serendipity Care Supports Families and Individuals
At Serendipity Care, we understand the challenges families face when supporting a loved one with schizophrenia. Our mission is to provide a safe, caring, and supportive environment that empowers individuals to reach their full potential. Through our residential homes, supported living accommodations, and domiciliary care services, we offer comprehensive, person-centred care based on the recovery model.
Our team works closely with families, commissioners, and healthcare providers to ensure that both mental and physical health needs are met. By creating a homely, nurturing atmosphere, we aim to support each person’s journey toward stability and growth. Together, we can build a brighter future for individuals living with schizophrenia and their loved ones.
If you’d like to learn more about our services, please reach out to us today. Let’s walk the path of recovery, side by side.
List of resources:
https://livingwithschizophreniauk.org/
https://www.nhs.uk/mental-health/conditions/schizophrenia/living-with/
Highlights from January 2025
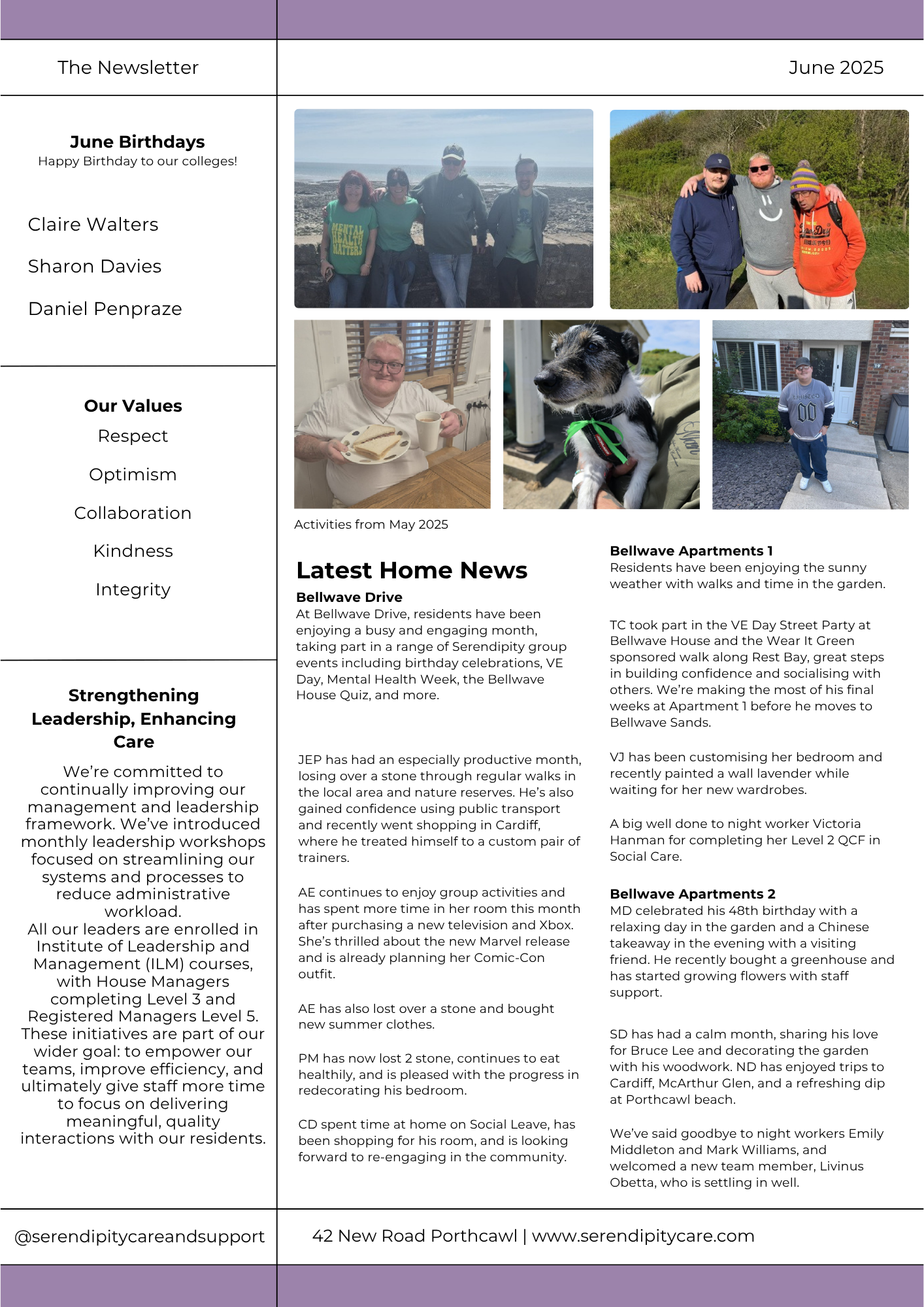
Sponsors of local club
We are thrilled to announce that Serendipity Care and Support are now the proud main sponsor of Mynydd Cynffig ABC, a local gym dedicated to promoting strength, discipline, and wellness in our community.
This sponsorship reflects our commitment to supporting active, healthy lifestyles and fostering a strong sense of community.
New role for Dionne Parry

Dionne Parry
A big congratulations to Dionne Parry who has taken on a new role as Assistant Finance / Admin.
Dionne joined Serendipity in August 2022 after gaining experience in Supported Living Services. With a Level 3 diploma in holistic therapies, she values the supportive environment.
In her new role as Admin Finance/Office Assistant, Dionne enjoys greater work-life balance and time with family. She looks forward to completing AAT training and further developing her skills.
Staff Spotlight

Paiton Clarke
Meet Paiton Clarke, our new Psychologist Assistant. Since joining Serendipity in 2019 as a 17-year-old office administrator, she has earned a First-Class BSc in Criminology and an MSc in Psychology.
With experience supporting victims of domestic violence and working with paediatric clinical psychologists, Paiton is committed to social justice and mental health.
Latest Home News
Bellwave House
January has been a time of renewed hope and energy for both residents and staff. Our regular events have been well-attended, with the quiz continuing to be a highlight for many.
To mark ‘Blue Monday,’ known as the most depressing day of the year, residents and staff gathered for a walk along Porthcawl beach. We took time to enjoy each other’s company over coffee, sharing positive conversations and discussing ways to support mental well-being.
The day was a reminder of how important it is to stay connected and engage in activities that uplift our spirits.
At Bellwave House, one resident, WS, has made remarkable progress in gaining independence. After moving in from a locked rehabilitation home just four months ago, WS has now been assessed as ready to transition to supported living.
He recently toured his new home at Bellwave Sands with House Manager Hannah Clifton and was impressed by the property, looking forward to this next chapter in his journey.
Bellwave Apartments 1
TC has begun a Managing Anxiety course with Adult Learning Wales and TC has found it to be highly beneficial. He is applying the insights gained to better manage his own experiences.
VJ has been enjoying her regular outings, which include shopping trips and nature walks.
Bellwave Apartments 2
Apartment 2 has been full of fun with Mario Kart tournaments and “Fakeaway Fridays,” where residents take turns cooking healthy meals like curries and pasta.
ND is back to football after the break and recently visited Old Trafford with activity co-ordinator Mark Williams, fulfilling a lifelong dream.
SD has been teaching guitar to Mark and other residents. He’s excited for his birthday trip to Cardiff and an AC/DC tribute show in February.
MD is settling in well, enjoying a trip to Porthcawl, improving his cooking, and playing Mario Kart. He’s also having friendly football banter with ND as a Liverpool fan!
Bellwave Drive
At Bellwave Drive, residents joined a Blue Monday walk along the Porthcawl seafront, spending time with others from different projects and finishing off with hot drinks. It was a great way to lift everyone’s spirits.
JEP celebrated his 21st birthday with a party at the Drive, featuring music, quizzes, plenty of food, and a birthday cake.
He had a wonderful time and expressed his gratitude to everyone who came to celebrate with him.
AE enjoyed the Blue Monday walk and has embraced the new year with regular walks, sauna visits, and swimming. She also participated in a group session on online safety, led by local police, a mental health nurse, and an OT.
PM is off to a good start this year, setting weight-loss goals by incorporating small walks and dietary changes.
He’s also been keeping active around the house and garden and enjoyed preparing Sunday lunch for himself and the other residents.
Bellwave Cottage
Lee-Ann Evans has joined the Cottage as the new activities coordinator.
MB is back at Slimming World with a positive mindset, enjoying friendly competition with Lee-Ann. He continues to thrive in his volunteering role, helping with collections and deliveries, and has started a journal to reflect on key moments and maintain well-being.
PW has had a great start to the year, spending quality time with his dad over three-course meals and taking part in the Blue Monday event with friends, enjoying coffee and a beach dog walk.
TM is focusing on healthy eating and a new routine. He works out weekly with MB at the gym and pool, with both supporting each other in cooking meals. TM also continues his maths and English studies at the Bridge Hub.
 Bellwave Corner
Bellwave Corner
We’ve beaten the “January Blues” at the Corner with plenty of nature and beach walks!
This month was full of celebrations. We marked JEP’s 21st birthday at Bellwave Drive, and MF and NW celebrated their 51st and 41st birthdays on January 19th with a meal at Wetherspoons.
NL enjoyed a fun trip to the park, while DW bravely got his nose pierced. DW has also been busy cooking meals like cottage pie and stew and creating a journal to track his goals.
Highlights from December 2024
Christmas Celebrations
Over the Christmas season, our residents at Serendipity had a great time enjoying lots of fun activities together. Whether it was decorating the home, sharing stories over a warm cup of tea, or getting stuck into festive games, there was always something to look forward to.
What made it even better was having family and friends visit, filling the homes with laughter and love.
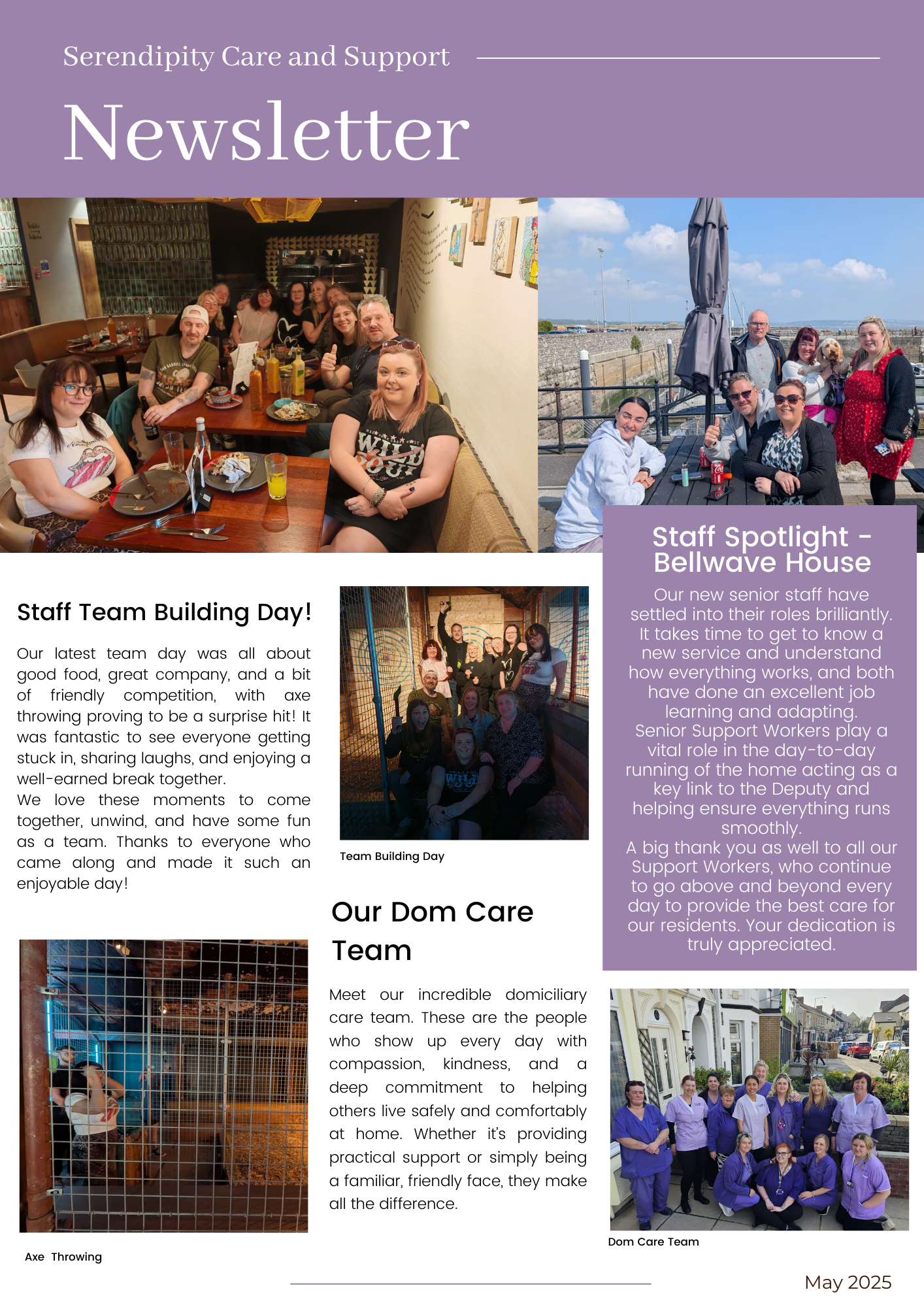
Employee of the Quarter

A big congratulations to our Senior Support Worker, Elisabeth James, on being awarded Employee of the Quarter! Since joining us in February 2024, Elisabeth has shown remarkable dedication and achieved so much.
Hayley and Mark would like to thank her for always going the extra mile—no task is too big or too small. Well done, Elisabeth, and thank you for being such a valued member of our team!
Latest Home News
Bellwave House
December was an exciting month for the residents of Bellwave House, made even more special by the festive Christmas and New Year activities.
A highlight was a Christmas meal at The Salt Water Inn, generously hosted by our RI, Tracy Wyllis, and the Serendipity Directors. Both residents and staff thoroughly enjoyed the experience, so a big thank you to Tracy and the Directors for making it possible.
Residents also participated in several enjoyable events throughout the month, including pumpkin picking, snow globe making, Christmas shopping in Swansea, and relaxing with tea and mince pies.
We are especially proud of our resident GW, who has made outstanding progress towards independence since arriving at Bellwave House. His psychiatrist has agreed to support him in regaining his driving licence, and GW is now planning to purchase a new van in the new year with hopes of returning to work as a plasterer.
This is a remarkable achievement, considering GW was previously in a low secure psychiatric facility before coming to Bellwave House.
Bellwave Cottage
It has been a busy and festive month at the Cottage, with residents enjoying Christmas shopping and a fun visit to Swansea Winter Wonderland with SD. Everyone who could make it gathered for a Christmas meal at The Red Dragon, a favourite among residents, and a great time was had by all.
The residents would like to thank everyone involved in their support for making this past year positive and rewarding.
TM spent Christmas with family, which was a wonderful experience, and is ready to start the new year with a positive outlook. PW and MB celebrated Christmas together, exchanging gifts, cooking a delicious lunch, and relaxing in front of the TV.
MB spent New Year’s Eve with his sister and her family, marking his first time celebrating away from the Cottage. Meanwhile, PW and TM welcomed in 2025 together.
Bellwave Drive
Residents at Bellwave Drive had a fantastic time preparing for the festive season, helping staff put up Christmas decorations and getting into the holiday spirit. They enjoyed completing their Christmas shopping for family and exchanged gifts with each other before heading home to celebrate with loved ones.
An afternoon was spent making personalised snow globes, which residents took home as keepsakes. They also gathered in the communal lounge to watch Christmas classics like Elf and The Grinch and shared a special evening watching the Gavin and Stacey finale.
A memorable event was the trip to Margam Park for the Luminate Lights. Residents, joined by Bellwave Corner and RI Tracey, enjoyed the stunning displays, interactive light games, and festive treats, including toasted marshmallows by the fire. The evening was a huge success, and they hope to visit again next year.
On Christmas Day, residents spent time with family and later shared stories about their day. They were delighted their gifts were well received and enjoyed the thoughtful presents they received in return.
Bellwave Apartments 1
Residents and staff at Bellwave Apartments 1 enjoyed the festive season with a Christmas meal at the Royal Oak and a lively party with a buffet and gift exchange. They also took part in Christmas Jumper Day, raising £50 for Dave the Children—a wonderful way to spread holiday cheer together.
Bellwave Apartments 2
It’s been a festive month at Apartments 2, where residents helped raise over £50 for Save the Children during Christmas Jumper Day. A joint Christmas party with Apartment 1 featured a buffet, festive treats, and gifts for everyone.
SD has been continuing with his guitar playing and performed during both the Christmas Jumper Day event and the party. ND is excited to visit Old Trafford to watch Manchester United, something he’s been looking forward to for a long time, and is eager to return to playing football in the new year. MD has settled in well, enjoying caring for his new fish and making homemade smoothies and milkshakes.
Bellwave Corner
All residents enjoyed the Christmas festivities, including shopping for presents. Most spent the holiday period with family, returning with fond memories. Residents also reflected on the year and completed their New Year’s resolutions. DW continues to enjoy weekly rock climbing sessions, gaining confidence with each visit.
Staff and residents shared a lovely Christmas meal at Cheetahs in Porthcawl, where Santa made a surprise appearance. DW and MF had a fun-filled day at Swansea Winter Wonderland, enjoying ice skating, bumper cars, games, and festive food. They also explored the Swansea National Waterfront Museum during their visit.
Physical Health and Schizophrenia
Introduction
When we think of schizophrenia, the focus often centres on its profound impact on mental health. However, this complex condition also significantly affects physical health, often in ways that go unnoticed.
People with schizophrenia are more likely to face physical health challenges than the general population, leading to reduced life expectancy, poorer quality of life, and an increased burden on healthcare systems.
In this article, we’ll explore the physical health risks associated with schizophrenia and discuss how an integrated care approach can improve outcomes for individuals living with the condition.
Physical Health Challenges in Schizophrenia
The Scope of the Problem
People with schizophrenia live, on average, 10 to 20 years less than those without the condition1. This striking statistic isn’t solely due to mental health struggles; physical illnesses are a major contributing factor. Research shows that over 75% of individuals with schizophrenia have at least one chronic physical condition, such as diabetes, cardiovascular disease, or respiratory disorders2.
These challenges often arise earlier in life compared to the general population. For example, individuals aged 25–44 with schizophrenia are five times more likely to experience heart problems than their peers3.
Common Physical Health Conditions

Obesity and Related Complications
Obesity is one of the most pressing health concerns for individuals with schizophrenia. Linked to poor diet, sedentary lifestyles, and the side effects of antipsychotic medications, weight gain often leads to other health problems like heart disease, diabetes, and certain cancers4.
Antipsychotics such as Olanzapine and Clozapine are known to cause significant weight gain, while newer medications like Aripiprazole and Asenapine have fewer effects on weight5. However, the issue isn’t solely medication-related; studies have shown that people with schizophrenia tend to consume diets higher in sugar and fat, with lower intake of fruits, vegetables, and fibre6.
Cardiovascular Disease

Heart disease and stroke are twice as common in individuals with schizophrenia as in the general population7. These conditions are exacerbated by smoking, poor diet, and inactivity, all of which are prevalent in this group.
Diabetes
Diabetes is more common among people with schizophrenia, with antipsychotic medications playing a potential role by altering the body’s use of insulin. Interestingly, outcomes for individuals in developing countries—where physical activity through farming or other labour is common—tend to be better, suggesting lifestyle factors like exercise may help mitigate risk8. Emerging research has also proposed a genetic link between schizophrenia and diabetes9.
Respiratory Disorders and Smoking
Approximately 70% of individuals with schizophrenia are smokers, compared to just 25% of the general population10. Smoking not only increases the risk of respiratory diseases but also interacts with medications, reducing their effectiveness and necessitating higher doses, which can worsen side effects like weight gain.
Bone Health
Conditions like osteoporosis are more prevalent in individuals with schizophrenia, linked to a sedentary lifestyle and, in some cases, elevated levels of the hormone prolactin caused by antipsychotics. High prolactin levels can weaken bones over time, making regular monitoring essential11.
The Role of Exercise in Schizophrenia
Exercise and Physical Health
Regular exercise plays a pivotal role in reducing the risk of chronic illnesses associated with schizophrenia. For instance:
- Heart Disease and Diabetes: Exercise is one of the most effective ways to reduce the risk of heart disease and diabetes, particularly for individuals with schizophrenia who are already at an increased risk due to lifestyle factors, medication side effects, and higher rates of obesity12. Regular physical activity helps the body regulate insulin levels, which is essential for controlling blood sugar and preventing type 2 diabetes. For people with schizophrenia, whose antipsychotic medications may alter the body’s ability to manage insulin effectively, this is especially important.
Moreover, exercise strengthens the heart muscle, improves blood circulation, and lowers levels of harmful cholesterol while increasing levels of “good” cholesterol. Even moderate aerobic activities such as brisk walking or cycling for 30 minutes a day, five days a week, can significantly reduce the likelihood of developing heart disease, regardless of weight loss12.
The benefits extend to reducing inflammation, improving arterial flexibility, and maintaining healthy blood pressure—all crucial factors in preventing cardiovascular issues. For individuals unable to engage in high-intensity workouts, low-impact exercises like swimming or yoga can still provide significant cardiovascular benefits without undue strain.
- Bone Health: Osteoporosis, a condition characterised by weakened bones, is more common in individuals with schizophrenia, particularly due to sedentary lifestyles and medication side effects11. Certain antipsychotics can elevate prolactin levels, a hormone that, when too high, can lead to reduced bone density over time. This risk, coupled with a lack of regular physical activity, creates a pressing need for targeted interventions to protect bone health.
Weight-bearing exercises, such as walking, dancing, and resistance training, are particularly effective in strengthening bones. These activities work by applying stress to the bones, which stimulates the bone-building cells and helps maintain or even increase bone density. Resistance training, such as using free weights or resistance bands, is especially beneficial as it combines muscle strengthening with joint stability, further reducing the risk of fractures.
- General Fitness: Regular physical activity is vital for improving overall fitness levels, which includes cardiovascular health, muscle strength, flexibility, and stamina12. For individuals with schizophrenia, who may lead more sedentary lives due to the negative symptoms of the condition (such as apathy and low motivation), even small increments in physical activity can have profound effects on physical and mental health.
Aerobic activities such as jogging, swimming, or cycling enhance cardiovascular fitness by strengthening the heart and lungs, which improves oxygen delivery throughout the body. This leads to reduced blood pressure and a lower resting heart rate—both markers of improved cardiovascular health.
Resistance training, including bodyweight exercises or gym-based strength training, boosts muscular strength and endurance. Stronger muscles support joints, improve posture, and enhance overall mobility, making daily tasks easier and less physically taxing.
Flexibility exercises, such as yoga or stretching routines, can improve joint range of motion, reduce stiffness, and minimise the risk of injury. Additionally, these exercises often provide mental health benefits, such as stress reduction and improved relaxation, which are particularly helpful for individuals with schizophrenia.
Exercise and Mental Health

The benefits of exercise extend beyond physical health, offering improvements in mental and psychological well-being:
- Negative Symptoms: Exercise has shown promise in alleviating negative symptoms like apathy, lethargy, and social withdrawal13.
- Cognitive Benefits: Some studies suggest exercise can enhance memory and cognitive functioning, although further research is needed13.
- Auditory Hallucinations: Anecdotal evidence indicates that exercise may help reduce the distress caused by hallucinations, possibly through distraction and focus14.
- Psychological Well-Being: Exercise is linked to reduced stress, better sleep patterns, improved self-esteem, and a greater sense of relaxation15.
Improving Physical Health Care
Proactive Monitoring and Intervention
Care homes and healthcare providers play a crucial role in bridging the gap between mental and physical health care. Regular health checks focusing on blood pressure, blood sugar levels, and heart health are essential. Early intervention in these areas can drastically improve life expectancy and quality of life.
Promoting Healthy Lifestyles
Encouraging physical activity, improving diet, and offering smoking cessation support are critical components of integrated care. For example, studies show that even modest increases in physical activity can significantly reduce the risk of heart disease and diabetes, regardless of weight loss12.
Tailored Medication Management
Where possible, prescribing antipsychotics with fewer metabolic side effects can help reduce weight gain and other associated health risks. Regular discussions with healthcare providers about side effects and medication adjustments are important5.
Holistic and Integrated Care Models
An integrated approach to care—bringing together mental health, physical health, and social services—ensures that individuals with schizophrenia receive comprehensive support. This includes not only managing health conditions but also addressing barriers to care, such as stigma and socio economic challenges16.
Conclusion
Schizophrenia profoundly affects both the mind and the body. By recognising and addressing the physical health risks associated with the disorder, care providers can help individuals live longer, healthier, and more fulfilling lives. At our care home, we are committed to supporting the whole person, ensuring that physical health is never overlooked.
If you’d like to learn more about how we approach integrated care for individuals with schizophrenia, please don’t hesitate to get in touch. Together, we can build a brighter future for those living with this challenging condition.
References
- Healthcare Quality Improvement Partnership, 2014, Second National Audit of Schizophrenia: What You Need to Know.
- Mitchell A, Malone D, 2006, Physical Health and Schizophrenia, published in Current Opinion in Psychiatry.
- Penedo F, Dahn J, 2006, Exercise and Wellbeing: A Review of Mental and Physical Health Benefits Associated with Physical Activity, published in Current Opinion in Psychiatry.
- Chesney E, Goodwin G, Fazel S, 2014, Risks of All-Cause and Suicide Mortality in Mental Disorders: A Meta-Review, published in World Psychiatry.
- De Hert M, et al., 2011, Physical Illness in Patients with Severe Mental Disorders, published in World Psychiatry.
- Peet M, 2004, Diet, Diabetes and Schizophrenia: Review and Hypothesis, published in The British Journal of Psychiatry.
- Lancet, 19th February 2011.
- Jurczyk A, et al., 2015, Beyond the Brain: Disrupted in Schizophrenia 1 Regulates Pancreatic β-cell Function via Glycogen Synthase Kinase-3β, published in The Journal of the Federation of American Societies for Experimental Biology.
- Fuller Torrey E, 2013, Surviving Schizophrenia, Harper Perennial.
- Faulkner G, Taylor A, 2005, Exercise, Health and Mental Health, Routledge.
- Warner R, 2000, The Environment of Schizophrenia, Brunner Routledge.
- Firth J, et al., 2015, A Systematic Review and Meta-Analysis of Exercise Interventions in Schizophrenia Patients, published in Psychological Medicine.
- Kimhy D, et al., 2015, The Impact of Aerobic Exercise on Brain-Derived Neurotrophic Factor and Neurocognition in Individuals With Schizophrenia: A Single-Blind, Randomised Trial, published in Schizophrenia Bulletin.
- Author’s personal experiences.
- Burton N, 2012, Living with Schizophrenia, Acheron Press.
- Eaton W, et al., 2006, Association of Schizophrenia and Autoimmune Diseases, published in The American Journal of Psychiatry.
Highlights from November 2024
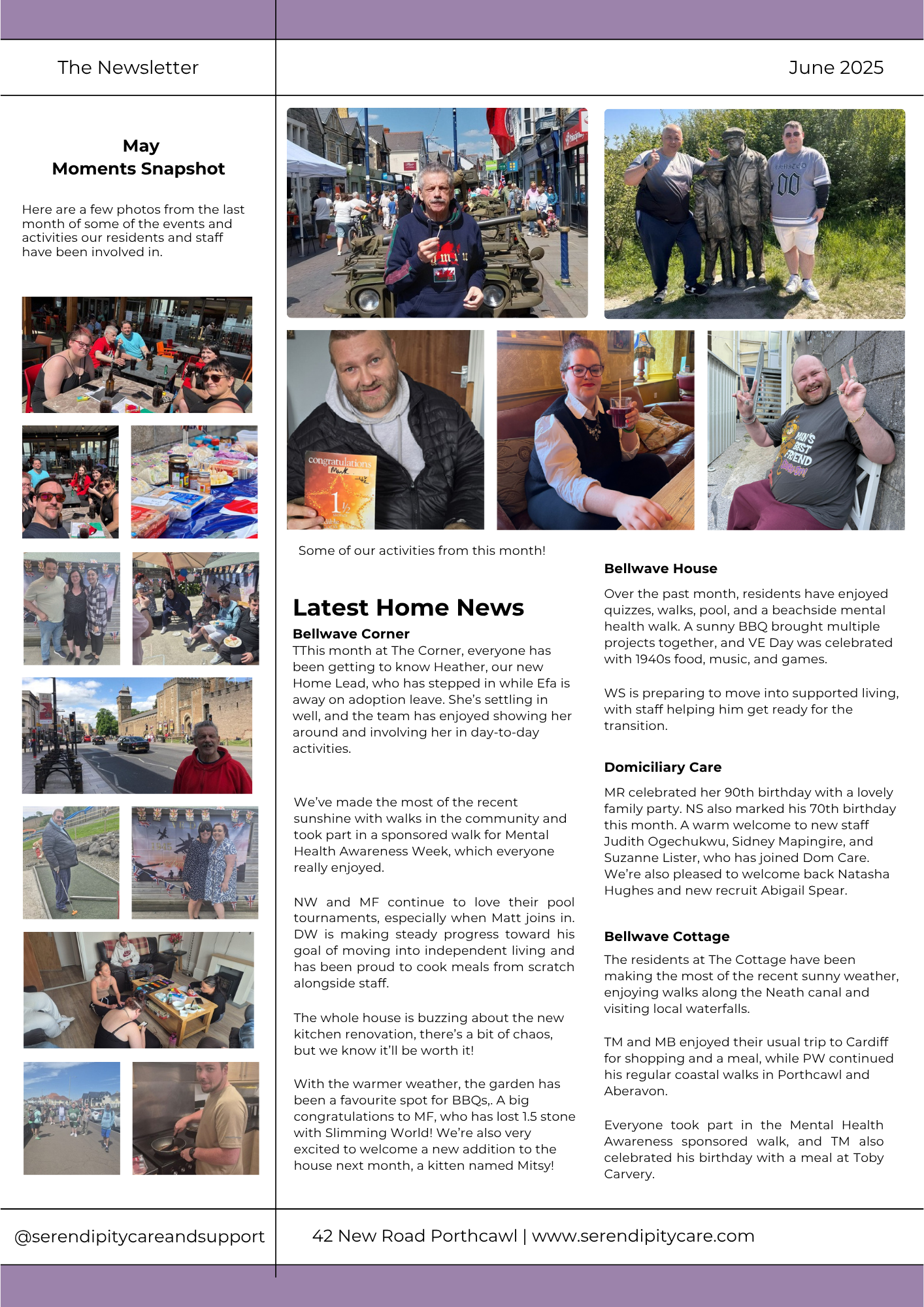
Recent Staff Forum
At Serendipity Care, our recent staff forum provided a valuable opportunity to reflect on our core values, company culture, and communication practices together.
It was an engaging session that reinforced our shared commitment to upholding the values that define Serendipity Care and ensuring open, effective communication across all levels of our organisation.
Staff Spotlight
Over the past month, Bellwave House has warmly welcomed three new staff members, all of whom are settling into their roles seamlessly.
Our new team leader, Shane Edwards, has also been finding his stride in the position. Reflecting on joining the team, Shane shared, “I’ve felt truly welcomed by both residents and staff, and I’m excited to take on the challenges ahead.”
We’re grateful to DW and NW for their fantastic support during recent interviews.
Their involvement brought valuable perspectives to the process, and their contributions were greatly appreciated.
In between interviews, they enjoyed some downtime watching The 1% Club and were treated to a chippy lunch as a small thank-you for their efforts.
Their assistance was greatly appreciated!
Bellwave House
Over the past month, residents at Bellwave House have enjoyed a mix of regular activities and special celebrations.
Bonfire Night was a highlight, with sparklers, coffee, and cake bringing everyone together for a cosy evening. Regular activities like pool and quizzes also kept spirits high throughout the month.
November was a month of celebrations, including birthdays for AD and AH, both of whom enjoyed a treat of a chippy lunch to mark their special days.
Our newest resident, WS, has been settling in exceptionally well. Since his arrival, he has grown much more comfortable in his new surroundings and is engaging with staff more actively. One of WS’s favourite routines is going out daily with staff for breakfast, which he thoroughly enjoys. It’s wonderful to see him feeling at home!
 Bellwave Corner
Bellwave Corner
It’s been a busy and engaging month at The Corner as we celebrated several National Days together. National Kindness Day saw us playing a kindness quiz, sharing kindness tips, and pulling names from a jar to say something kind about each person.
On National Play Monopoly Day, we embraced the spirit of the day by enjoying a lively game of Monopoly.
For National Stop Violence Against Women Day, we learned important facts and played games like “Guess the Female Lead Film” and “Guess the Celebrity,” focusing on women who have survived violence or domestic abuse.
MF and DW also attended a Mental Health First Aid Course at the YMCA in Porthcawl. Both found the experience educational and rewarding.
Meanwhile, Christmas spirit has arrived early at The Corner! We’ve started putting up decorations, and while some might say it’s a bit soon, everyone here is fully embracing the festive mood.
Looking ahead, we’re planning a Christmas shopping trip, a visit to Winter Wonderland, and plenty of other holiday activities to keep the celebrations going!
Bellwave Drive
It’s been another busy and exciting month for all residents, filled with a variety of activities. Amelia has fully embraced the festive spirit, enjoying decorating gingerbread houses and listening to Christmas songs.
She also welcomed a new pet hamster, Athena, who has settled in wonderfully in her bedroom. Amelia has been growing more confident each day and is clearly enjoying her time with Athena.
PM and JEP have also been getting into the Christmas spirit, enjoying shopping for gifts and spending time choosing presents for their families and loved ones. The festive cheer is truly in full swing!
 Bellwave Apartments 1
Bellwave Apartments 1
Our new resident, TC, has been settling in wonderfully. He’s been enjoying exploring the community, both independently and with support from staff.
This month, apartment residents also participated in Road Safety Week, organised by our Activities Coordinator, Victoria. She put together a quiz to test everyone’s road safety knowledge, which was both fun and informative!
Bellwave Apartments 2
It’s been a settled and enjoyable month at Apartments 2. We welcomed a new resident, MD, who is settling in wonderfully and already planning to get some pet goldfish to make his space feel more like home.
This month, we also said goodbye to our fantastic Support Worker and Activity Coordinator, Dionne Parry, who has moved to a new role in the office. Dionne will be greatly missed, but we wish her all the best in her new position.
ND has started attending street football again and is thoroughly enjoying being back in the game.
SD continues to delight in playing his guitar and immersing himself in music. He recently enjoyed a trip to Cardiff for some shopping and a visit to the music store. SD has also been busy creating customised jackets featuring his favourite bands.
With Christmas just around the corner, we’re all excited about the upcoming festivities and activities to celebrate the season!