Jennifer Cosslett
Understanding Domiciliary Care: A Flexible Alternative to Residential Care
Introduction
Making decisions about care is often far from straightforward. Whether you are thinking about support for yourself or for someone you love, the process often brings a complicated mix of practical concerns and emotional weight.
Domiciliary care offers an alternative that challenges those assumptions. Rather than asking someone to adapt to a care setting, care is brought to them, into the place they already know and feel safe. For many individuals across the UK, this approach provides the right balance of support, dignity, and independence.
This article explores what domiciliary care is, who it can benefit, and why it has become such a valued option for so many families. It will also explain why the quality of the care provider matters, and how the right support can make a meaningful difference to everyday life.
What Is Domiciliary Care?
Domiciliary care, sometimes referred to as home care, is support provided to an individual in their own home. It is designed to help people manage daily living while remaining in familiar surroundings, rather than moving into a residential care setting.
The support provided through domiciliary care can range from short visits once or twice a day to more regular and involved assistance, depending on a person’s needs. Care is delivered according to an agreed care plan, which is created following an assessment and reviewed regularly to ensure it continues to reflect the individual’s circumstances.
Crucially, domiciliary care is not about taking over someone’s life. Assessments focus on what a person can already manage independently, and support is added only where it is needed. The aim is to maintain health, safety, dignity, and wellbeing while encouraging independence wherever possible.
Domiciliary care can be arranged through local authorities or privately through care providers. In both cases, the core principle remains the same. Care should be personal, respectful, and tailored to the individual, recognising that everyone’s needs, preferences, and home environments are different.
Who Can Benefit from Domiciliary Care?
Domiciliary care supports a wide range of people, not just those who might traditionally be associated with care services. It is suitable for anyone who needs help with daily living but wishes to remain at home and retain as much independence as possible.
Older adults are one of the most common groups to benefit. Many people reach a point where everyday tasks become more challenging, even though they are otherwise mentally sharp and socially engaged. In these cases, a small amount of well-timed support can make the difference between coping and thriving, allowing individuals to stay connected to their routines, memories, and communities.
People with physical disabilities or mobility challenges may also benefit from domiciliary care. Support can be tailored to specific needs, helping individuals move safely around their home, manage personal care, or access the outside world without unnecessary restrictions.
Domiciliary care can also support individuals with learning disabilities or mental health needs. Familiar surroundings often provide a sense of security and stability that cannot be replicated elsewhere.
Additionally, domiciliary care is frequently used on a short-term basis. People recovering from illness, surgery, or a hospital stay may need temporary support while they regain strength and confidence.
What Services Does Domiciliary Care Typically Include?
Domiciliary care services are highly flexible and can be adapted to suit individual needs, lifestyles, and circumstances. There is no standard package, because no two people live or age in the same way.
Personal care is often a core element. This may include help with washing, dressing, using the toilet, or getting in and out of bed. Delivered with sensitivity and respect, personal care should always preserve privacy and dignity, recognising that these are deeply personal aspects of daily life.
Medication support is another common area of assistance. This might involve reminders, supervision, or practical help to ensure medication is taken safely and as prescribed. For many people, this reassurance alone can significantly reduce stress and health risks.
Care workers may assist with meal preparation, ensure regular eating, or help someone maintain a balanced diet that suits their preferences and needs.
Domiciliary care can also include help with light household tasks such as cleaning, laundry, or shopping. While these may seem small, they are often the first things to become overwhelming. Addressing these early can prevent greater difficulties later.
Equally important is companionship. Care visits are often a valued source of conversation, reassurance, and human connection. For many people, knowing someone reliable will arrive, listen, and care makes a significant difference to their emotional wellbeing and sense of security.
The Advantages of Domiciliary Care
One of the most significant advantages of domiciliary care is the ability to remain in a familiar environment. Home is more than just a physical space. It holds memories, routines, personal belongings, and a sense of identity. Being able to stay at home often provides comfort, stability, and emotional security that cannot be replicated elsewhere.
Maintaining independence is another key benefit. Domiciliary care supports people to live life on their own terms, with assistance added only where it is genuinely needed. Independence does not disappear when care begins, within domiciliary care, it is actively protected.
Care delivered at home is also inherently more personal. Unlike residential settings, where staff must divide attention between many people, domiciliary care is typically one-to-one. This allows care workers to build genuine relationships and understand not just a person’s needs, but their preferences, habits, and personality.
Domiciliary care can also be more flexible than residential care. Support can increase or decrease as circumstances change, whether temporarily or long term. This adaptability means care can grow alongside someone, rather than forcing major life changes at the first sign of difficulty.
For many families, cost is also a consideration. While care needs and circumstances vary, domiciliary care can often be a more cost-effective option than moving into a residential care home, particularly when full-time support is not required. More importantly, it allows resources to be focused on meaningful, personalised care rather than institutional overheads.
Addressing Common Concerns About Care at Home
Despite its many advantages, families often have understandable concerns about domiciliary care. One common worry is safety. People may fear that living at home could increase risks, particularly if someone’s health or mobility is declining. In reality, well-planned domiciliary care is built around risk awareness and prevention, with assessments and care plans designed to keep individuals safe while preserving independence.
Some people worry that receiving care at home could be isolating. However, for many individuals, moving away from their home and community can be far more disruptive. Domiciliary care allows people to maintain existing relationships with neighbours, friends, and family, while also benefiting from regular contact with care workers who provide companionship and reassurance.
Finally, families often worry about reliability and consistency. This is a valid concern, and it highlights why the choice of provider is so important. A high-quality provider prioritises communication, continuity, and respect, ensuring care feels supportive rather than intrusive.
Why Choosing the Right Provider Matters
While domiciliary care offers many benefits, the experience depends a lot on who delivers it. The difference between care that feels supportive and care that feels stressful often comes down to the values, culture, and practices of the provider.
High-quality domiciliary care is person-centred, meaning care is shaped around the individual rather than squeezed into rigid schedules or checklists. This requires time, training, and a genuine commitment to understanding the person behind the care plan.
Consistency is also crucial. Seeing familiar faces builds trust, reduces anxiety, and allows care workers to notice subtle changes in health or mood. A good provider prioritises continuity wherever possible and communicates clearly when changes are unavoidable.
Equally important is communication with families. Domiciliary care works best when everyone involved feels informed, listened to, and confident that concerns will be taken seriously. Care should feel like a partnership, not a service delivered in isolation.
Choosing the right provider means choosing an organisation that values dignity, respects choice, and understands that care is about people first and processes second.
Domiciliary Care with Serendipity Care & Support
At Serendipity Care & Support, domiciliary care is built around the understanding that no two people experience life, or need support, in the same way. Care is tailored, flexible, and designed to fit naturally around the individual rather than forcing change or disruption.
Each person receives a personalised care package shaped around their specific needs, routines, and preferences. This may include personal care, practical support, or companionship, delivered by a dedicated carer who provides continuity and reassurance throughout the care journey. Familiar faces and trusted relationships are central to how Serendipity delivers care.
Care plans are created with real life in mind. Existing routines are respected, whether that involves medication schedules, preferred daily rhythms, or meaningful hobbies. Plans remain flexible over time, adjusting as circumstances change so that support always remains appropriate, responsive, and respectful.
Alongside personal care, Serendipity offers domestic support to help ease the pressures of everyday living. From household tasks and meal preparation to errands and practical assistance, these services are designed to reduce stress and support independence, allowing people to focus their energy on living well.
Additional support is also available where needed, including family support, informal carer relief, specialist care, and access to a 24 hour on call service. Throughout all aspects of care, the emphasis remains the same. Dignity, choice, and wellbeing come first.
Serendipity’s approach is rooted in compassion, professionalism, and a genuine commitment to putting people at the centre of their care. The goal is not simply to meet needs, but to support individuals to live comfortably, confidently, and with dignity in the place they call home.
Conclusion
Domiciliary care offers a flexible, respectful, and empowering alternative to residential care for many individuals and families. By allowing people to remain in their own homes, it preserves independence, identity, and emotional wellbeing while providing essential support.
When delivered well, care at home is not a compromise. It is a positive choice that adapts as life changes and places dignity at the centre of every interaction. The right care, delivered in the right way, can transform everyday life.
With a thoughtful, person-centred approach, domiciliary care enables people to continue living in the place they love, supported, respected, and understood.
Highlights From October 2025
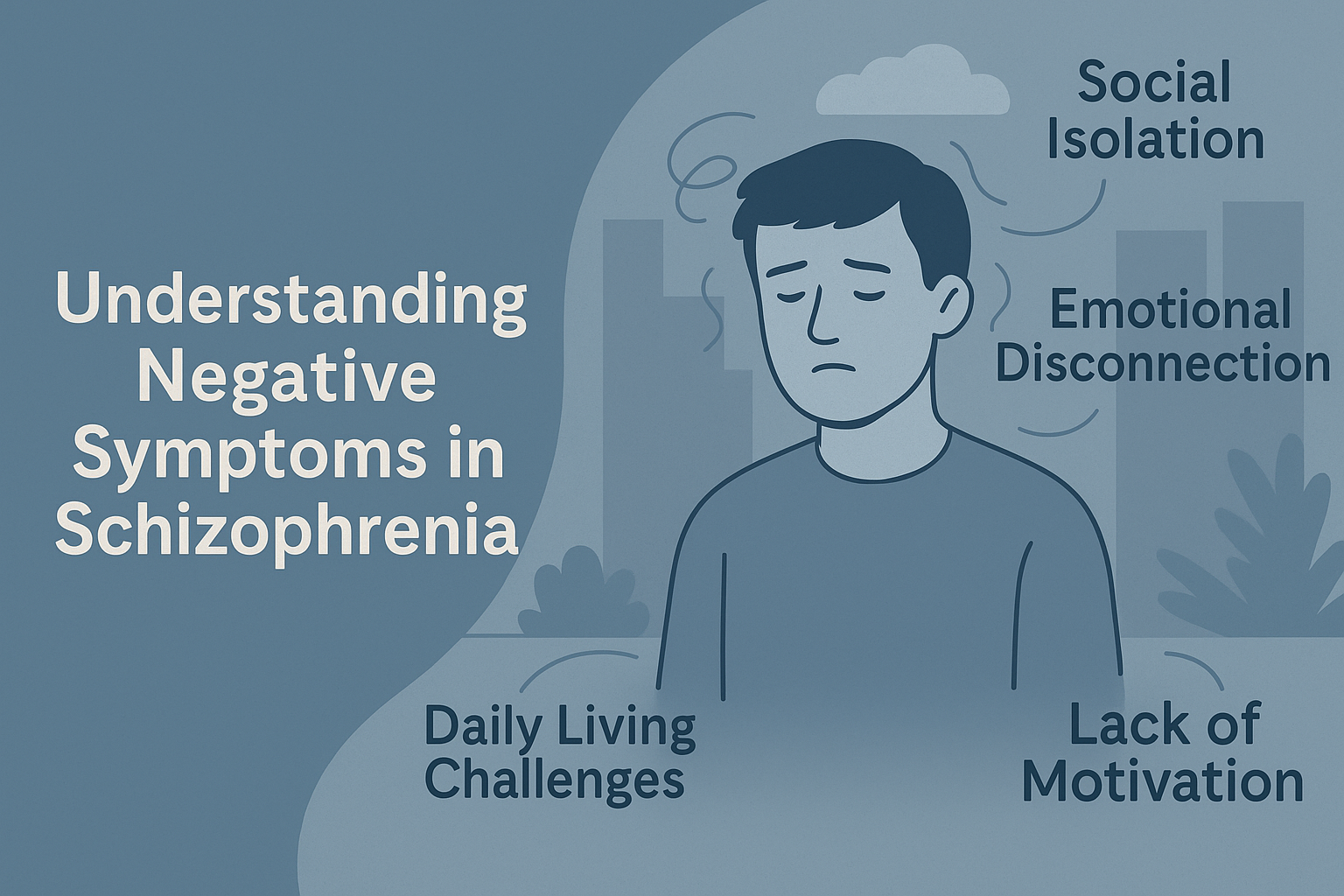
Understanding Negative Symptoms in Schizophrenia
Introduction
When most people hear the word schizophrenia, their minds immediately jump to dramatic symptoms often portrayed in films and media. Hallucinations, or delusions for example. These are known as positive symptoms, and while they can be distressing, they’re often treatable with medication.
Before we continue, with the context of this article’s topic in mind, the words “Positive” and “Negative” do not mean “Good” and “Bad”. Instead they carry the meaning more like “Additive” and “Subtractive”.
What many people don’t know is that schizophrenia also brings another set of challenges, ones that are far less visible but often more disabling in the long run. These are the negative symptoms. Unlike positive symptoms, which add experiences that shouldn’t be there (like hearing voices), negative symptoms involve the loss of normal abilities and behaviours.
For families, carers, and even professionals, these symptoms can be confusing and frustrating. Why does your loved one seem withdrawn? Why don’t they want to do things they once enjoyed? Why do they seem emotionally “flat”? Understanding these questions is key to providing the right support.
What Are Negative Symptoms?
Negative symptoms refer to the absence or reduction of typical behaviours, emotions, and motivations that are essential for daily functioning. They are not about being “negative” in attitude but about missing aspects of normal mental and emotional life.
Unlike the dramatic and visible nature of positive symptoms such as hallucinations, these changes are subtle and often misinterpreted as laziness or lack of interest. In reality, they stem from complex neurological processes that impact motivation, reward, and emotional regulation.
Here are the main categories:
- Affective Flattening – A noticeable reduction in emotional expression. The person might speak in a monotone voice, show little facial expression, or seem “blank” even during emotionally charged moments.
- Alogia – Limited speech. Conversations become short and minimal, not because of rudeness, but due to difficulty generating thoughts or expressing them.
- Anhedonia – Loss of pleasure in activities that used to bring joy. Even favourite hobbies or social outings may hold no appeal.
- Avolition – A lack of motivation to initiate or sustain activities. Everyday tasks like showering, cooking, or tidying up can feel overwhelming.
- Asociality – Withdrawal from social interactions. Relationships may fade because engaging with others feels exhausting or pointless.
These symptoms are not a choice. They reflect deep changes in brain functioning that make previously simple tasks feel like climbing a mountain. Unfortunately, their subtle nature means they’re often overlooked by family, friends, and even healthcare providers.
Recognising them early is key to offering the right support, building realistic expectations, and creating an environment that encourages small, sustainable steps toward engagement and recovery.
Why Are Negative Symptoms Misunderstood?
Unlike hallucinations or delusions, negative symptoms aren’t obvious. They don’t make headlines or feature in dramatic TV scenes. Instead, they look like “quiet suffering.” This invisibility leads to misinterpretation and stigma.
Many families mistake these symptoms for laziness or apathy:
- “He just doesn’t care anymore.”
- “She’s being antisocial.”
In reality, negative symptoms stem from neurological disruptions in areas of the brain responsible for motivation, reward, and emotional processing. Think of it like a car with an empty fuel tank: the engine (the person) is still there, but there’s no energy to make it move.
Negative symptoms are also commonly confused with depression or side effects of medication. While overlaps exist, they are distinct issues requiring different strategies. Unfortunately, this misunderstanding often delays effective intervention, leaving the individual and their family frustrated and disconnected.
Impact on Daily Life
The effect of negative symptoms can be profound and far-reaching. Unlike positive symptoms, which may come and go, negative symptoms often persist over time and quietly erode a person’s quality of life.
These changes ripple outward to families, friendships, and work environments. While positive symptoms might draw attention due to their disruptive nature, negative symptoms often hide in plain sight, gradually dismantling routines and relationships.
Here’s how they commonly manifest:
- Social Isolation – Friends drift away. Conversations become rare. Loneliness sets in. What once felt effortless—chatting over coffee, attending gatherings—becomes an exhausting mental task.
- Daily Living Challenges – Hygiene, cooking, cleaning—all can fall by the wayside, not out of choice but due to lack of mental energy and motivation. Even something as small as brushing teeth can feel overwhelming.
- Employment Difficulties – Holding a job becomes difficult when motivation and focus are diminished. Tasks pile up, and performance issues may be misread as disinterest rather than symptoms.
- Emotional Disconnection – Loved ones may feel shut out because emotional warmth seems absent. Smiles, laughter, and shared moments fade, creating misunderstandings and tension.
These struggles can be devastating. Many individuals desperately want to engage with life, but their internal resources simply aren’t there. This disconnect often leads to feelings of guilt, frustration, and hopelessness, compounding their mental health challenges.
Families, too, can feel helpless or even resentful, not realising that these behaviours aren’t a choice. Understanding the true nature of negative symptoms is the first step toward offering compassion and practical support that can make a real difference.
Why Are They So Hard to Treat?
Medication, while life-changing for positive symptoms, often does little for negative symptoms. Antipsychotic drugs primarily target dopamine pathways involved in hallucinations and delusions, but negative symptoms involve broader brain networks affecting motivation, pleasure, and cognition.
Current research explores new medication options and therapies, but for now, psychosocial interventions remain the backbone of treatment. This includes structured routines, behavioural activation (gradually reintroducing rewarding activities), and skills training.
How Residential Care Can Help
This is where dedicated residential support changes lives. Negative symptoms thrive in environments lacking structure and encouragement. In contrast, care homes like Serendipity create predictable, supportive routines that reduce stress and gently promote engagement.
Some key strategies:
- Structured Daily Routines – Predictability is calming and helps reduce decision fatigue. Having consistent meal times, scheduled activities, and gentle reminders creates a sense of order that can anchor individuals who might otherwise feel adrift.
For someone struggling with avolition, knowing what comes next can be the difference between completing a task and avoiding it altogether.
- Engagement Activities – Activities like art, gardening, or cooking groups provide stimulation in a non-threatening way. These go beyond hobbies, and offer a sense of accomplishment and rekindle interest in the world.
When carefully chosen and introduced at the right pace, such activities can bypass the weight of apathy and spark small moments of joy or curiosity.
- Supportive Social Opportunities – Traditional social situations can feel overwhelming for someone with negative symptoms. Low-pressure group interactions, such as a shared tea break or collaborative art session, allow social skills to rebuild gently.
The goal isn’t forced participation but creating safe, welcoming spaces where connection feels possible without pressure.
- Skilled Observation – Negative symptoms often shift slowly, making it easy to miss early signs of improvement or decline. Staff trained to notice subtle changes like a slight increase in eye contact, a willingness to join a group, or conversely, a retreat into isolation, can adapt care plans before issues escalate. This attentiveness is vital for long-term stability and progress.
The goal isn’t to force participation but to create opportunities for success. Small wins that rebuild self-esteem and motivation are the goal.
How Families Can Support Loved Ones
Family support is vital, but it requires understanding and patience. Here are practical tips:
- Avoid Criticism – Comments like “Try harder” or “You’re being lazy” are harmful. Negative symptoms are not a choice. Criticism can deepen feelings of shame and withdrawal, making recovery even harder.
- Encourage Small Steps – Instead of “Let’s go out for the day,” try “Would you like to sit in the garden for 10 minutes?” Starting small helps build confidence and prevents the person from feeling overwhelmed.
- Celebrate Progress – Even tiny improvements matter. Acknowledge them warmly. Positive reinforcement can motivate further engagement and show the person that their efforts are valued.
- Maintain Connection – Even when responses are minimal, your presence and consistency provide security. Silent companionship can still offer comfort and reduce feelings of isolation.
- Seek Education – Learn about negative symptoms to adjust expectations and reduce frustration. Understanding the condition helps caregivers respond with empathy rather than impatience.
Why This Matters
Negative symptoms can be more disabling than positive symptoms. They erode quality of life and independence and can strain relationships to breaking point. Without targeted support, these symptoms often persist for years.
At Serendipity Care, we understand that supporting someone with schizophrenia isn’t just about controlling psychosis—it’s about nurturing the whole person. Our homes provide structured, compassionate environments where individuals can stabilise, reconnect, and rediscover meaning in life.
If you’d like to learn more about how we support people with complex mental health needs, contact us today. Together, we can build a future where no one faces this silent struggle alone.
Highlights from September 2025
Highlights from August 2025
Highlights from July 2025
Highlights from June 2025
Highlights from May 2025
Highlights from April 2025